Last November, as part of our work to help all of you who have been touched by chordoma live your best lives before, during, and after treatment, we hosted Living Well: Caring for yourself during stressful times, a 60-minute webinar outlining strategies and tips for self-care.
Featured speakers

Susie Rinehart
Mom, leadership coach, international girls’ empowerment advocate, ultrarunner, author of Fierce Joy, and chordoma survivor (diagnosed in 2016)

Amy Bragman, LCSW
Licensed Clinical Social Worker at The University of Texas MD Anderson’s Brain and Spine Center
Watch the recording
If you weren’t able to join us for the webinar, we encourage you to watch the recording. We heard from a number of attendees who found it very valuable and we hope you agree.
Key takeaways
We had the opportunity to share Susie Rinehart’s story last fall, and welcomed her insightful and poignant suggestions during the Living Well webinar. Diagnosed with chordoma in 2016, Susie has had three craniotomies, a neck fusion, months of radiation, and experimental systemic therapy. Through her role as a leadership coach, international girls’ empowerment advocate, and author of Fierce Joy, she has developed and trained others on a number of self-care tools for managing the physical and emotional hurdles that arise in life. During her chordoma journey, she has applied these tools to face down her own challenges with boldness and optimism.
Susie’s tips:
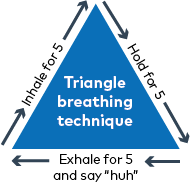
Breathe through your stress. Your breathing can have a significant impact on how you feel. Susie taught us how to do the 5-5-5 breathing exercise sometimes referred to as a triangle breath. Using this technique, you breathe in for 5 seconds, hold for 5 seconds, and then breathe out of your mouth for 5 seconds. We learned that the keys to an impactful 5-5-5 breath are to hold in the middle for the full 5 seconds and make a “huh” sound as you exhale. This technique stimulates the vagus nerve and tells your body to rest and relax.
Create a 3-2-1 plan. The next strategy that Susie shared was a 3-2-1 plan for dealing with particularly stressful times. She walked us through how to write our own plan and suggested having it easily accessible to use as a guide during particularly stressful times. Your 3-2-1 plan should include:
- 3 people who lift you up. These should be impactful people in your life who may not be part of your daily life but with whom you can connect when you’re feeling stressed and need a supportive boost.
- 2 places you can go to support your mind and your mood. During stressful times, going to one of these places can help you clear your mind and lift your mood. These can be a physical place (e.g., park, nature trail) or someplace you go in your mind (e.g., beach, mountaintop).
- 1 thing that kicks you out of spinning thoughts and into a place of resiliency and strength. This could be baking, music, exercise, or any pleasant activity that helps you settle your thoughts.
Notice the difference between clean and dirty pain. Did you know there are two types of emotional suffering? Neither did we! Susie taught us about this idea, explaining that events which cause emotional distress — such as receiving a cancer diagnosis, the death of a loved one, losing a job — are types of clean pain. The emotions we feel are a normal, natural response to something that has happened to us.
Dirty pain is caused by the thoughts and judgements we have about those events, like “I should have…”, “what if…”, or “things are never going to get better”. Susie encouraged us to try to notice when we feel dirty pain, recognize it for what it is, and observe it without judgment. Then, turn our attention to what has caused these thoughts instead (the clean pain), and let it motivate us to be kind to ourselves. This mindset requires daily calibration but can be very impactful. Susie shared that during her recovery from chordoma treatments, she made purposeful choices focused on loving and giving, rather than fearing or taking.
You may recognize our second speaker, Amy Bragman from our 2018 Chordoma Community Conference at MD Anderson Cancer Center where she is a Licensed Clinical Social Worker with the Brain and Spine Center. Amy is also featured in the videos How can caregivers and loved ones help? and What support is available for mental and emotional health needs? from our Expert Answers Series.
Amy reminded us that feelings of anger, irritability, and guilt are normal for chordoma patients and their family members. A cancer diagnosis and the treatment that follows are shared traumas for both patients and their caregivers. It’s okay to allow yourself time to adjust and important to learn new coping strategies because we can’t always control the outcome, but we CAN control how we react.
Amy’s tips:
Connect with others. Resilience isn’t just about surviving, it’s about thriving and finding the benefits of what has happened. It’s about how you come back. Amy encouraged us all to look for opportunities for social engagement such as volunteering, actively listening to people we care about, and performing random acts of kindness. These connections can improve our ability to be resilient.
Get moving. She reminded us about the importance of moving and getting outside regularly to help increase hormones like endorphins that make us feel good. Exercising, eating well, and getting plenty of sleep all sound simple, but they impact our emotions and that is why they are important to self-care. Similarly, she discussed how journaling, meditation, and mindfulness are beneficial for calming our entire bodies.
Give back. “Finding a way to give back or find a sense of purpose is so important. It helps us make sense,” shared Amy. “Nothing makes sense about cancer. You will drive yourself crazy trying to make sense of it. Try to embrace the changes and find a sense of purpose in the experience.”
Regardless of what strategies and techniques you choose for self-care, it is important to take time to focus on your overall well-being throughout your chordoma journey. For more specifics, we encourage you to watch the full webinar!
Chordoma Foundation resources
Several Chordoma Foundation resources were discussed during the webinar. We put together a quick list as a helpful reference:
Patient Navigation Service
If you or someone you love has been diagnosed with chordoma, Chordoma Foundation Patient Navigators are here to help you get the best care possible.
Peer Connect
Support from someone who has been there can make all the difference. Peer Connect is a free, confidential peer-to-peer support program that connects anyone touched by chordoma with another person whose experiences with chordoma are similar.
Chordoma Connections
Our private online community, Chordoma Connections, is a place for chordoma patients and their loved ones to ask questions, share updates, learn about research advances, and connect with others around the world. Join today!
Chordoma Survivorship Survey
In order to learn more about the issues you’re facing, the resources that have helped, and how the Foundation can assist in better meeting your needs, we have developed a survey focused on chordoma survivorship and quality of life. Whether you are a patient or survivor, caregiver or family member, or you have lost someone you love to chordoma — we want to hear from you.
The survey is now closed. View the preliminary results.
Natural History Study of Rare Solid Tumors
The chordoma community is one of a number of rare cancer communities that has been invited to participate in this study, currently underway at the U.S. National Cancer Institute (NCI). The purpose of this important study is to collect clinical and biologic information including tumor tissue samples from patients anywhere in the world with rare solid tumors, such as chordoma, to better understand how these tumors develop and grow. By taking part in this Natural History Study you can help speed the identification and development of new treatments by giving researchers the information they need to make progress.
E-newsletter signup
To stay up-to-date with the Chordoma Foundation, please subscribe to our emails. You will receive relevant updates about research progress, treatment advances, educational resources and events, and opportunities to get involved.
Information provided by the speakers in the Living Well webinar is not medical advice. Please follow up with your doctor to discuss the information you learn from this webinar.