Get support
Our Patient Navigators can provide more information on managing side effects.
Managing challenges with vision, hearing, speech and swallowing, pain, endocrine function, balance, and sinuses. About 30 percent of chordomas form within the center of the head in an area called the skull base – usually in a bone called the clivus.
The clivus is next to the brainstem and both carotid arteries, in an area containing nerves that control important functions such as vision, hearing, speech, and swallowing. Clival chordomas can sometimes involve the upper bones of the cervical spine as well. In most cases, surgery is recommended as the first treatment for tumors in these areas, and radiation therapy is generally recommended after surgery to kill any remaining tumor cells.
People with clival (skull base) or upper cervical chordomas who have undergone surgery and/or radiation sometimes experience side effects and quality of life challenges in the months or years following treatment. These include:
These side effects are typically caused by compression of the cranial, C1, or C2 nerves as a tumor grows or nerve damage that occurs as a result of surgery and radiation. They can also be caused by damage to the glands of the endocrine system or to the soft tissues of the sinuses and throat.
The Chordoma Foundation is a resource for anyone affected by chordoma, at any stage of your journey. We're here to help you understand the disease, its side effects, find qualified doctors, and connect with others in the chordoma community.

The clivus is a bone at the base of the skull. The top two bones of the cervical spine are called the C1 (Atlas) and C2 (Axis) vertebrae. The Atlas supports the brain. It is the gateway between the skull and spine, protecting and providing a path for the central nervous system to connect the brain to the body. The Axis allows the head to pivot.
All of these bones are part of the craniovertebral junction (CVJ), where the head and neck meet
and the brain transitions to the spinal cord.

Cranial nerves come in pairs. There are 12 pairs of cranial nerves that emerge directly from the brain and provide motor and sensory functions to the head and neck. The nerves are named for the functions they control and are also referred to by number -- for example, 6th cranial nerve.
1. The olfactory nerves are critical for the sense of smell and are some of the few nerves capable of regrowing.
2. The optic nerves relay messages from the retina of the eye to the brain to create visual images.
3. The oculomotor nerves help control muscle movements of the eyes, including the constriction of the pupil, and keep the eyelid open.
4. The trochlear nerves are also involved in eye movement and control the eye muscles that are responsible for rotation, allowing the eye to point downward or inward.
5. The trigeminal nerves are the largest and most complex cranial nerves. They are responsible for sensation and motor function in the face and mouth, enabling a person to chew or clench their teeth. Each trigeminal nerve splits into three branches, controlling the feeling for different parts of your face:
- The ophthalmic branch → eye, upper eyelid, and forehead
- The maxillary branch → lower eyelid, cheek, nostril, upper lip, and upper gums
- The mandibular branch → jaw, lower lip, lower gum, and some muscles used for chewing
6. The abducens nerves control the eye muscles that are responsible for lateral movement, enabling the eye to turn its gaze outward.
7. The facial nerves have both motor and sensory functions. They control muscles that help you make expressions like raising an eyebrow, smiling, or frowning. They are also responsible for most of the tongue’s taste sensations.
8. The vestibulocochlear nerves, also called the acoustic nerves, are responsible for hearing and balance.
9. The glossopharyngeal nerves provide motor and sensory information to the mouth and throat. Among their many functions, these nerves help raise part of the throat, enabling swallowing.
10. The vagus nerves are the longest cranial nerves, running from the brain through the face and thorax to the abdomen. They are responsible for many tasks, including heart rate, muscle contractions that move food through the digestive tract (peristalsis), sweating, and muscle movements in the mouth, including speech and keeping the larynx open for breathing.
11. The spinal accessory nerves control specific muscles of the shoulders and neck.
12. The hypoglossal nerves control the tongue movements of speech, food manipulation, and swallowing.
Like the cranial nerves, spinal nerves also come in pairs. The nerves emerge from the spinal cord and exit through small openings between the vertebrae. There are seven cervical vertebrae, but eight pairs of cervical spine nerves labeled C1 through C8. They stimulate muscle movement in the neck, shoulders, arms, and hands. The C1 and C2 nerves control the forward, backward, and side-to-side movements of your head and neck.
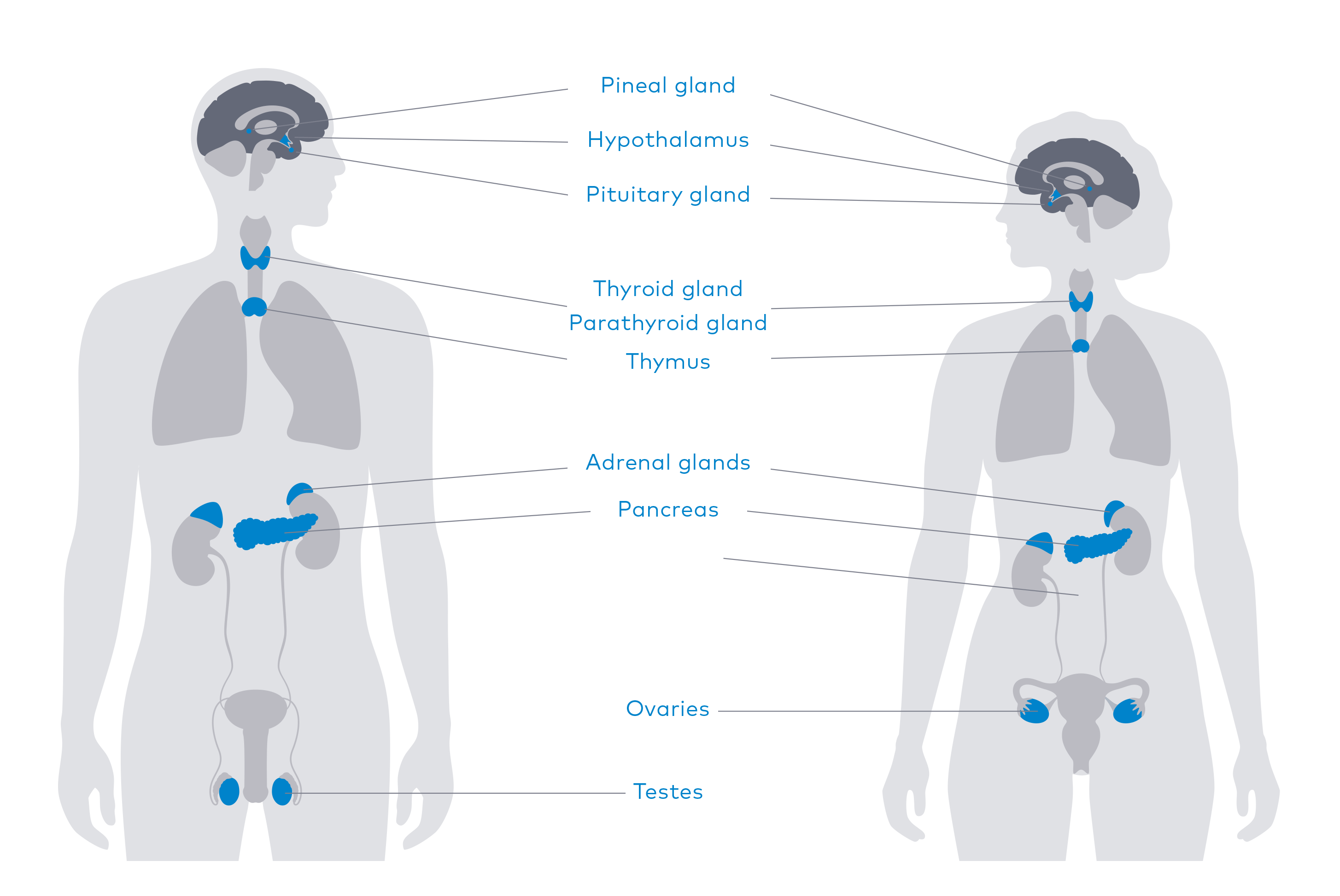
The glands that make up the endocrine system influence reproduction, metabolism, growth, and many other functions. They are located throughout the body, with many in the head and neck. These include the hypothalamus, pituitary, thyroid, and parathyroid glands. Each of these glands is responsible for producing specific hormones.
Hormones are chemicals that act as the body’s communication system, coordinating different functions by carrying messages through the blood to organs, skin, muscles, and other tissues. These signals tell your body what to do and when to do it.
The hypothalamus is a gland deep within your brain. It is the main link between your endocrine system and your nervous system. Your hypothalamus keeps your body balanced in a stable state called homeostasis.
The pituitary is divided into two main sections: the anterior pituitary (front lobe) and the posterior pituitary (back lobe). The primary function of the pituitary gland is to produce and release hormones that help carry out important bodily functions, including growth, metabolism, reproduction, and more.
The thyroid releases hormones that control the way your body uses energy. The thyroid’s hormones regulate vital bodily functions, including breathing, heart rate, body weight and temperature, muscle strength, cholesterol levels, and more.
The parathyroid produces a hormone that plays a crucial role in regulating calcium levels in the blood. Precise calcium levels are important in the human body as small changes can cause muscle and nerve problems.
Treatment provided by doctors and teams specializing in chordoma can significantly improve outcomes for individuals with clival and upper cervical chordomas. However, because chordomas are located near vital nerves, organs, and arteries, treatment is often complicated and, in some cases, can lead to serious side effects.
Before you begin treatment, ask your doctors about the risks and what side effects are possible or likely, to ensure you are comfortable with the treatment plan.
Assessment and treatment will depend on what you’re experiencing but should always begin with a complete and thorough evaluation of your current symptoms and your chordoma treatment history. To make sure your doctor is prepared for your visit, be sure to have your medical records sent to their office before your appointment.
The sections below discuss side effects often experienced by people with clival and upper cervical tumors and possible treatments.
If you are experiencing any of the issues in this list for the first time or they are suddenly getting worse, let your doctors know. New or worsening symptoms can be a sign of new tumor growth, or they may be late effects of treatment as described above.
|
Types |
Causes |
Tests |
Specialists |
|---|---|---|---|
|
Double vision, strabismus, blurred vision, loss of vision, loss of depth perception |
Typically caused by compression of or damage to 2nd-6th cranial nerves from tumor growth, surgery, or radiation. |
Vision tests — such as a neuro-ophthalmology evaluation — are usually done before chordoma treatment to establish a baseline and should be done again after treatment to compare and track progress. |
Neuro-ophthalmologist and/or ophthalmologist |
An ophthalmologist is a medical doctor who can diagnose and
medically or surgically treat eye problems and diseases. A neuro-ophthalmologist specializes in vision problems related to nervous
system function, making them the ideal type of doctor to help
address visual side effects caused by a clival or upper cervical tumor.
A neuro-ophthalmologic exam is one of the most comprehensive types of medical evaluations. It can take a few hours to complete. Here are some things to know:
Depending on your specific symptoms, treatment may include:
|
Types |
Causes |
Tests |
Specialists |
|---|---|---|---|
|
Hearing loss, tinnitus (ringing in ears) |
Typically caused by damage to or compression of the 8th cranial nerve (acoustic) during tumor growth, surgery, or radiation. |
Tests that should be done before chordoma treatment include hearing tests such as a physical exam of the ear, an audiogram, a brainstem auditory evoked response (BAER), or imaging. If there is hearing loss after treatment, similar tests should be conducted, and the results should be compared. |
Audiologist |
Conductive hearing loss is when something blocks your outer or middle ear, stopping sound from reaching your inner ear.
Sensorineural hearing loss is when something damages your inner ear or the nerve that connects your ear to your brain.
It is the type of hearing loss most commonly experienced by chordoma survivors, and it often happens only on the side with the damaged nerve – known as unilateral hearing loss.
Mixed hearing loss is when both conductive and sensorineural loss are present.
Tinnitus is when you experience ringing or other noises in one
or both of your ears. There are two main types of tinnitus, subjective (when only you hear the sounds) and objective (when a doctor can hear the sounds you hear).
Hearing loss that results from chordoma tumor growth or treatment can be immediate or gradual. If caused by radiation, you may not have symptoms until many years later. Symptoms include:
Depending on the cause of hearing loss, treatment may include:
Medical treatment such as ear drops, ear wax removal, or surgery
Vestibular therapy for vertigo or dizziness issues
Assistive devices such as hearing aids, implants, or sound generators
Counseling techniques like Acceptance and Commitment Therapy (ACT) or Cognitive Behavioral Therapy (CBT)
Lifestyle changes such as modifications to diet, sleep, or exercise

There are a few clival survivors who lose their sense of smell after treatment. This is called anosmia and can be caused by damage to the 1st cranial (olfactory) nerves. When anosmia is caused by nerve damage it may or may not be possible to treat it. An otolaryngologist is the type of doctor who treats anosmia. Lifestyle changes, such as learning new ways to cook, can sometimes help.
|
Types |
Causes |
Tests |
Specialists |
|---|---|---|---|
|
Dysarthria (difficulty with speech), Dysphagia (difficulty swallowing) |
Most often caused by compression or damage to the 9th (glossopharyngeal), 10th (vagus), and/or 12th (hypoglossal) cranial nerves as a result of tumor growth or treatment. Other causes include cervical spine hardware or radiation necrosis that affects the tissues of the esophagus. |
For dysarthria, your doctor might order tests to identify underlying conditions, such as imaging tests, brain and nerve studies, blood and urine tests, and neuropsychological tests. For dysphagia, you may undergo imaging tests, swallowing studies, endoscopy, or an esophageal muscle test. |
Speech-language pathologist Otolaryngologist (ENT) |
Weakness or issues controlling the muscles of the tongue, lips, vocal cords, or diaphragm can cause problems with speech. Symptoms include:
Dysphagia is the subjective sensation of difficulty swallowing. Types of dysphagia are specific to which part of your swallowing action — beginning a swallow (oropharyngeal dysphagia) or completing it (esophageal dysphagia) — is affected. In both cases, symptoms of dysphagia include:
Whether you have difficulty with speech, swallowing, or both, the following treatments may help:
|
Types |
Causes |
Tests |
Specialists |
|---|---|---|---|
|
Headaches, neuropathy, trigeminal neuralgia (TN) |
The trauma of surgery can cause swelling in the head which can in turn cause a headache. If headaches were a symptom of chordoma for you, expect them to be a symptom after treatment for a period of time. Other head and facial pain can be caused by damage to the 5th (trigeminal) or 7th (facial) nerves. |
The main assessment for headaches and facial pain are the patient’s reports of their symptoms. Doctors will consider your medical history, do a physical examination, and complete special investigations, if needed. Trigeminal neuralgia is diagnosed by excluding other conditions that might be causing the symptoms. |
Neurologist, pain specialist, primary care physician |
Headaches are common when clival tumors are growing and begin to cause symptoms. Following surgery, headaches may continue while your body recovers. Nerve damage can cause pain, tingling, and numbness in your scalp, face, or neck. It can also affect your ability to move some of the muscles in your face, causing facial paralysis. These symptoms may resolve after treatment, or they may continue for months or years. They may also worsen over time if caused by radiation.
Trigeminal neuralgia (TN) has been described as the most excruciating type of pain. It most often occurs on one side of the face only, typically in the lower face and jaw but can sometimes be felt around the nose and eye. If left untreated, trigeminal neuralgia can progressively worsen.
The pain from TN is separated into two types, TN1 and TN2, due to different types of symptoms. People can experience both types at the same time.
TN1
|
Types |
Causes |
Tests |
Specialists |
|---|---|---|---|
|
Adrenal insufficiency, growth hormone deficiency, hyperprolactinemia, hyper/hypothyroidism, diabetes insipidus, low estrogen/testosterone |
Most often caused by radiation-induced damage to the organs of the endocrine system located in the head and neck. 30-50% of patients with tumors in the skull base will develop hormone deficiencies after radiation. |
Your doctor should evaluate you using blood tests at the time of diagnosis to determine if there are any existing hormone imbalances. If there are, treatment will likely be recommended to bring them under control before surgery or therapy. Testing should be done again about 6 weeks after surgery — before you start radiation — and every 6 months to a year after that, indefinitely. |
Endocrinologist or neuro-endocrinologist |
When an endocrine gland isn’t functioning properly, it can’t produce hormones the way it should. The glands in the system are all connected, so if one gland in the head or neck isn’t producing
hormones normally, it can affect the function of glands in other parts
of the body.
An endocrinologist is a medical doctor who can diagnose and treat hormone imbalances. Some endocrinologists focus specifically on the interaction between the nervous system and the endocrine system. These doctors are sometimes referred to as neuro-endocrinologists. They are very well suited to treat hormone imbalances in chordoma survivors, but all endocrinologists can provide this treatment.
Symptoms can appear soon after radiation treatment but are more likely to start a few years later, which is why it’s very important to undergo regular testing of your hormone levels. Symptoms depend on which hormones aren’t being produced and can include:
Medication or a combination of medications to help balance hormone levels is the main treatment for endocrine issues. Some medications you may be taking for other reasons can mimic hormone deficiencies, so be sure to keep careful track of all your medications and provide them to your neuro-endocrinologist

These are common questions asked by chordoma survivors.
Adrenal and pituitary deficiencies can be life-threatening so
these should always be treated. Thyroid imbalances can also
safely be treated. However, there isn’t enough evidence to
know for sure whether replacement growth hormone or sex
hormones (estrogen, testosterone, etc.) will affect chordoma
growth. Determining whether to treat these deficiencies
should be done in careful consultation with both your
chordoma team and a neuro-endocrinologist, taking risks
and quality of life into consideration.
|
Types |
Causes |
Tests |
Specialists |
|---|---|---|---|
|
Balance impairment, vertigo or dizziness, loss of mobility |
Often caused by a number of the challenges addressed above, such as double vision, vision loss, vertigo, or dizziness. Balance issues can also be caused by medications or deconditioning (loss of physical fitness). |
You should be assessed for any balance and mobility issues at the beginning of your treatment and at regular intervals during and after treatment with tests such as balance and proprioception evaluation, posturography, vision tests, nerve conduction studies and sensory tests, laboratory tests, and imaging tests. |
Physiatrist, physical therapist, occupational therapist, vestibular rehabilitation therapist |
Treatment should address the cause of your specific balance issues, and can include:
|
Types |
Causes |
Tests |
Specialists |
|---|---|---|---|
|
Mucus buildup, crusting or dripping, bleeding from nose, irritation or infection (characterized by redness, tenderness, heat, or puss) |
Surgery through the nose (endonasal or transsphenoidal) or the mouth (transoral) can require soft tissue reconstruction and/or create scar tissue. This can lead to abnormal mucus production and irritation. |
Your doctors will examine your nasal passages, sinuses, and throat both before and after surgery. |
Otolaryngologist (ENT) |

Depending on the particular side effects you are experiencing, you may need to speak with more than one specialist to address them. Your care team may include rehabilitation therapists, neuro-endocrinologists, otolaryngologists, neuro-ophthalmologists, and others.
It is sometimes possible to schedule visits with specialists at the center where you were treated for chordoma. For instance, if you see your chordoma team in-person for follow-up visits, ask for referrals to other specialists in the medical center and make appointments to see the specialists while you are there for follow-up. You can then ask the specialist to consult with a specialist local to you so they can plan and follow your treatment together.
If you can’t be seen by a specialist at the center where you were treated, ask your chordoma care team for referrals in your local area. Some chordoma doctors will do consultations with local specialists, even if you haven’t seen them in person.
Seek out specialists at your nearest academic medical center. These
specialists will likely not have experience with chordoma, and that’s
okay. You and your chordoma care team can help educate them on
chordoma and your experiences with it.
Palliative care is an important part of cancer care. Sometimes called supportive care, it is recommended for all cancer patients from the time of diagnosis, through all stages of treatment, and after treatment is complete. It can address symptoms of the disease itself or side effects of its treatment.Chordoma experts recommend that all chordoma patients’ treatment plans and survivorship care plans include palliative care. No matter what treatment you have for chordoma, palliative care can help address pain, mobility and functional issues, mental and emotional health, nutrition, fatigue, and many other concerns to help you feel well and live fully while managing your chordoma.
Read more about palliative care
To help you find specialists to address the side effects of treatment, we created a Survivorship Specialist Directory within Chordoma Connections, our online community. It is a supplement to our Doctor Directory, an invaluable tool on our website you can use to locate surgeons, radiation oncologists, and medical oncologists who have extensive experience treating chordoma.
The Survivorship Specialist Directory allows chordoma community members to share information about providers who have helped address quality of life concerns, including pain specialists, urologists, rehabilitation therapists, and more.
Search the Survivorship Specialist Directory in Chordoma Connections
Many care providers who can help you manage side effects won’t know a lot about chordoma. And that’s okay. The Chordoma Foundation developed a fact sheet you can use to help your doctors, nurses, and other healthcare providers learn about chordoma. It includes general information on chordoma, how it’s treated, and the common side effects of those treatments. There is also space for you to add information about your situation so your providers can understand how chordoma has affected you personally. Share this fact sheet with your providers to help them learn about chordoma.
If you are caring for someone with clival or upper cervical chordoma who is experiencing side effects, there are a number of things to keep in mind and ways you can support them. Remember that if they are dealing with more than one type of side effect, they may require the care of multiple types of doctors and specialists. It can be a lot to keep track of. Things you can do include:
Help schedule and manage doctor’s visits, writing down a list of questions to ask at each appointment beforehand.
Find a good cadence of checkups with different doctors and specialists, making sure the number and timing of appointments is manageable and that information is being shared across the care team, such as care instructions and medication lists.
Watch for worsening side effects, particularly after changes in your loved one’s care plan or periods of higher stress.
Consider adjusting your living environment to accommodate your loved one’s side effects. This could mean lowering or raising the volume on TVs or stereos, preparing food a certain way, or removing items that may be tripping hazards.
Get support for yourself as well. Seeing your loved one experience ongoing challenges can be emotionally and psychologically taxing, and having someone to talk to can make a big difference.
Chordoma Foundation Patient Navigators provide personalized information and support to anyone affected by chordoma, anywhere in the world, at any stage of their journey. Your Patient Navigator will use their extensive knowledge of chordoma to help answer your questions, provide information about treatment guidelines, help you find qualified doctors, talk with you about side effects, and connect you with others in the chordoma community who have been through a similar journey.
The information provided herein is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your or your child’s physician about any questions you have regarding your or your loved one’s medical care. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.